There is a large unmet clinical need for the early detection of sepsis in patients with or developing sepsis. The detection of sepsis is frequently delayed, which can lead to delays in treatment. Earlier administration of sepsis-specific treatments, particularly antibiotics, is associated with improved clinical outcomes, including significantly reduced mortality. Lack of sepsis recognition is one of the common causes of its misdiagnosis and contributes to adverse outcomes due to delays in definitive antimicrobial treatments.
What is Monocyte Distribution Width?
Monocyte Distribution Width (MDW) is an in vitro diagnostic parameter that reflects a change in the volume of circulating monocytes in response to pro-inflammatory signals from infectious organisms—referred to as pathogen-associated molecular patterns (PAMPs).

Figure 1. The Pathophysiology of Sepsis.
What Analytical Systems Can Provide MDW?
The MDW parameter is available as a part of the complete blood count (CBC) with white blood cell (WBC) differential (CBC-Diff) hematology analysis using Early Sepsis Indicator application* within 2 hours from whole blood venous sample collection.

Figure 2. Hematology analyzer reporting MDW parameter.
What is the Intended Use of the MDW Parameter?
The regulatory-cleared MDW in vitro diagnostic (IVD) parameter is intended for use with adult patients presenting to the emergency department, on whom a white cell differential test has been ordered.
MDW is measured from a (K2EDTA) whole-blood venous sample within 2 hours of collection. MDW values greater than 20.0 together with other laboratory findings and clinical information, aids in identifying patients with sepsis or at increased risk of developing sepsis within the first 12 hours of hospital admission.
MDW values greater than 20.0 should be interpreted in association with other clinical information and diagnostic testing, as a proportion of patients without sepsis may have an elevated MDW value at baseline.
MDW values less than or equal to 20.0 cannot rule out sepsis or the development of sepsis within 12 hours of hospital admission. The Early Sepsis Indicator should not be used as the sole basis to determine the absence of sepsis.
The predictive value of the Early Sepsis Indicator for identifying sepsis in patients with hematological abnormalities has not been established.
Moreover, the results are automatically available as part of the CBC-Diff results with no impact to laboratory or emergency department workflow and no incremental cost per patient.
How is the MDW Parameter Measured?
During the CBC-Diff, each of the WBC cell types is characterized in their near-native state to generate a 5-part differential (neutrophils, eosinophils, monocytes, lymphocytes, and basophils) that includes both cell number and proportion.
When there is an infection or inflammatory process in the body, the bone marrow releases more WBCs into the blood. Monocytes and neutrophils represent the first line response during an infection. The accompanying inflammatory process may result in their activation leading to morphological and functional changes.
These morphological changes, even the slight ones, are detected by the proprietary near-native state characterization capability.
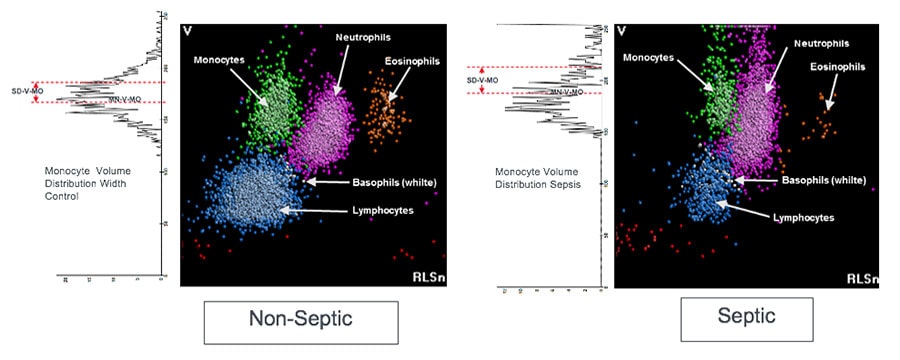
Figure 3. Cell population distribution analysis. Representative histograms of WBC populations. (Left) Example of a nonseptic donor. (Right) Two-dimensional histogram corresponds to an example of a patient with septic shock. Crouser et al. 2017.
Why Should Clinicians Use It?
There is a large unmet clinical need for the early detection of patients having or developing sepsis.
Emergency departments have initiated measures to detect sepsis as early as possible, but a reliable biomarker of sepsis has not been available.
Existing biomarkers of sepsis such as procalcitonin (PCT) and lactate are typically ordered only if the clinician already has a high index of clinical suspicion of sepsis. The most critical unmet needs are the identification and alert of sepsis (when the physician does not of sepsis from Systemic Inflammatory Response Syndrome (SIRS).
Resources to Support Your Efforts
MDW has been studied for the past decade with more than 16 peer-review publications and over 21,000+ patients,1-10 confirming the robustness and reproducibility of MDW performance in different patient populations.
Explore educational resources to support your hospital and labs efforts to overcome the challenges of identifying sepsis.

 English
English





